The Other Battlefield: Surge in Opioid Use Among Wounded Gaza Soldiers
They were injured on the battlefield and received painkillers for their injuries. However, during the rehabilitation process, some soldiers discovered that withdrawing from the medications was a battle of its own. Experts working to prevent a wave of addicted wounded soldiers warn that without proper support, they could spiral into street drugs. A Shomrim investigation, published also in Yedioth Ahronoth 7 days supplement


They were injured on the battlefield and received painkillers for their injuries. However, during the rehabilitation process, some soldiers discovered that withdrawing from the medications was a battle of its own. Experts working to prevent a wave of addicted wounded soldiers warn that without proper support, they could spiral into street drugs. A Shomrim investigation, published also in Yedioth Ahronoth 7 days supplement

They were injured on the battlefield and received painkillers for their injuries. However, during the rehabilitation process, some soldiers discovered that withdrawing from the medications was a battle of its own. Experts working to prevent a wave of addicted wounded soldiers warn that without proper support, they could spiral into street drugs. A Shomrim investigation, published also in Yedioth Ahronoth 7 days supplement
One of the soldiers interviewed for the article. Photo: Shlomi Yosef

Daniel Dolev
June 6, 2025
Summary


Listen to a Dynamic Summary of the Article
Created using NotebookLM AI tool
The rooms in the rehabilitation center at Sheba Medical Center in Tel Hashomer have balconies overlooking a lush lawn. They are filled with IDF unit insignias and stickers commemorating the soldiers who have fallen since October 7. Alongside the relatives and friends who come to visit, officers also mingle with the patients being treated for their wounds – many of whom are soldiers themselves and are starting to discover that their injury was just the opening salvo in a long battle with hospitalization, rehabilitation and a lot of pain. At the same time, they’re also exposed to another critical battle—less visible and far less talked about: preventing addiction.
“I’ve taken almost every kind of painkiller there is,” says Eli – not his real name – who was a member of one of the infantry divisions that was deployed to try and push back the Hamas terrorists who invaded the Gaza envelope on October 7 and was wounded in battle. “Until now, I would take between 12 and 15 pills a day,” he says. “Anything that came in a pill form or a solution – I would take it. Half of them were for post-trauma and half for the pain. Lyrica, Percocet and a drop of Valium – that’s what I would take just for the pain.”
According to Eli, no one warned him that some of the drugs he was taking could be addictive and that he could become physically dependent on them. He found out the hard way. “If I forgot my pills when I left the house or even one of the four pills that I take in the evening, I wouldn’t know what to do with myself,” he recalls. “I would sit there and think about how to get home. Why do I not have the pills on me? How did I allow myself to get into this position? Why don’t I have any medicine with me? And then it sends you into a cycle whereby you can’t live without them. You start every morning by running to the box where the pills are stored.”
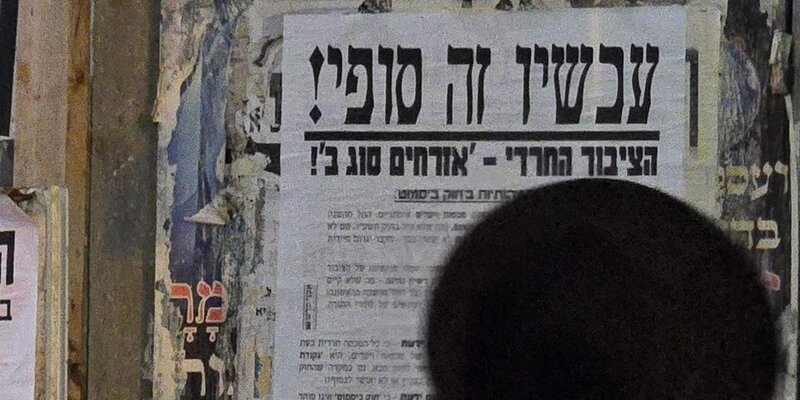
Eli recently decided to stop taking painkillers altogether. “Enough is enough, I told myself. I didn’t want to get to the stage when I was popping pills constantly; that could lead to an irreversible deterioration. There was a two- or three-week period when I really suffered; from the pain, the withdrawal symptoms – everything combined. Some days I sweated the whole day from pain or threw up; other days I was short of breath and things like that. I was totally jonesing. Now, I don’t even want to touch the pills. I saw what they did to me.”
Reservist Yuval – who also requested to use a pseudonym – was wounded in battle and has been undergoing rehabilitation since the early days of the war, after being injured during Israel’s initial ground incursion into the Gaza Strip. A gunshot wound to his leg caused severe nerve damage. “For the first two or three months, I constantly felt a current running through my leg,” he says. “It was like being electrocuted or stung. Imagine someone pressing a cattle prod to your leg and shocking you. Then sometimes, it felt like they’d come at you with pliers and squeeze hard, or grab your thumb. Or take a lighter and try to set your leg on fire.”
“During that period, I was given any drug you can possibly think of,” he says, before reeling off a list of the highly powerful pharmaceuticals he was prescribed: Tramal, Tramadex, morphine, Targin, Lyrica, Percocet, Valium shots and liquid Optalgin. Yuval says that he took Oxycodone, a particularly strong opioid, “at a later stage, during rehab. There was even a period when they brought me a special machine that I was hooked up to for three days. I got a shot of morphine at the press of a button. You’re hooked up to an IV, and every 20 minutes you get the option to press the button and receive a few milligrams of morphine.”
Many of the painkillers Yuval mentioned belong to the opioid family—powerful, highly effective medications, but also extremely addictive. In the past, they were used almost exclusively in emergencies or for terminal cancer patients. But since the 1990s illegal trade in the U.S. turned them into the source of a deadly epidemic, with hundreds of thousands of overdose deaths and millions of people addicted. Many of these addicts – who were first prescribed opioids by their physicians following surgery, some kind of injury, or chronic pain – eventually ended up consuming them without supervision via the black market, or even using street drugs like heroin.
In Israel too, the past two decades have seen a sharp rise in opioid use, especially among non-cancer patients under the age of 65. In 2021, Shomrim published a series of articles examining the opioid epidemic. According to HMO’s data, the increase leveled off in 2023, stabilizing at around 90,000 Israelis who received prescriptions for strong opioids—of which about 21,000 received them for more than six months.
There is now broad consensus that prolonged use of opioids inevitably leads to physical dependence—meaning that stopping the medication triggers withdrawal symptoms. Some patients will also develop addiction, which may manifest in neglecting responsibilities, work, or studies; damage to social relationships; inability to quit despite efforts; and more.
There are no official figures in Israel —or even an accepted estimate— regarding the number of drug addicts, let alone specific figures of those addicted to opioids. According to the 2022 State Comptroller’s Report, around 27,000 people addicted to drugs or alcohol are known to authorities and treatment providers. However, the Ministry of Welfare estimated that in reality, about 120,000 individuals are “somewhere on the addiction scale.” The report stressed that the state’s data “does not provide a full and up-to-date picture of the scope of drug and alcohol use.” A senior official in the Ministry of National Security, which oversees the Authority for Community Safety (formerly the Anti-Drug Authority), estimated this month that the real number is closer to 200,000 addicts.

‘If you make them go cold turkey, they’ll buy street drugs’
Eli and Yuval are not alone. Data obtained by Shomrim through the Movement for Freedom of Information in Israel regarding the use of opioids in rehabilitation centers in Israeli hospitals shows a worrying increase in the prescription of these pharmaceuticals since the outbreak of the war.
At the Sheba Medical Center in Tel Hashomer – the largest of the country’s rehabilitation hospitals - there was a sharp increase in the use of opioids in the immediate aftermath of October 7. In September 2023, the hospital prescribed 194 doses of Targin 20, which contains the opioid Oxycodone. Two months later, in November 2023, 632 of these pills were prescribed and by December 2023 the number had risen to 817. In total, 5,278 instances of opioids being prescribed to patients were recorded in Israeli rehabilitation hospitals, compared to 2,586 in September 2023. This is not a temporary increase, however; in December 2024 – more than a year later – 4,296 doses of opioids were prescribed.
Tel Aviv’s Ichilov Hospital has also seen a steady and significant rise. In 2022, the hospital’s rehabilitation unit ordered 899 doses of opioids from pharmacies. In 2023 – only the last 12 weeks of which were impacted by the war – the number skyrocketed to 1,146 and in 2024 it was even higher: 1,545 doses ordered. That represents an increase of around 72 percent compared to the pre-war figures of 2022.
One of the problems, according to Oren Miron, who has researched opioid use as part of his doctoral studies at Ben-Gurion University, as well as for the Clalit HMO and the Ministry of Health, is that with the types of wounds being treated, there is sometimes no alternative to opioids. “Sometimes it is just the initial treatment and sometimes it goes beyond that,” he says. “For many of the patients, physiotherapy can be so painful that the only thing that allows them to even move is a dose of opioids.”

Miron takes some cautious encouragement from the fact that it seems that the increase in opioid use mainly stems from moderate opioids, like low-dosage Oxycod, rather than far more potent drugs like Fentanyl patches, which are high-dosage drugs. At the same time, he adds, the more relevant question is what happens after the patient’s release from hospital. “Soldiers get very dedicated treatment from a highly skilled team at the rehab centers. The challenge becomes even harder when they get home, when the responsibility for the rehabilitation process is handed over to doctors from the HMOs’ rehabilitation units – so that they can ensure that the patients do not develop a dependency on the drugs and so that the GP knows what quantity of opioids the patients were taking at the rehabilitation hospital. They need to take note if the patient showed signs of distress and addiction; maybe they tried unsuccessfully to reduce the dosage because the patient showed signs of withdrawal.”
Yuval also believes that the moment the wounded soldier is sent home is a weak link in the chain. “There’s this thing called SOS, which is basically emergency pain meds,” he explains. “That means you’re not popping them daily, but if you get a severe pain attack, you take them. It could be cannabis, Optalgin, Tramadex, or Oxycod for me. When you head home from the ward for the weekend, they give you an exact number of syringes. But after you’re discharged, when you’re not in the rehab department anymore, if you’re eligible for those SOS meds, you can order them from the pharmacy. I could get liquid vials of Tramadex, for example, and the pharmacist would tell me how much I should take. But in practice, no one’s stopping me from downing a bottle of Tramadex a day if I feel like it.”
A year ago, Yuval underwent neurosurgery which significantly reduced not only the intensity of the pain but also the frequency – and he says that he gradually reduced his consumption of opioid painkillers until he eventually stopped using them altogether. He still takes Lyrica, a non-opioid medication primarily used to manage nerve pain and anxiety.
“It's crucial to remember that no matter how cautious you are, there will be instances where it will lead to addiction, necessitating treatment and interventions because these opioids are highly addictive substances,” Miron warns. “So, we must exercise caution when tapering doses; we must not panic and stop in one fell swoop. Because if you make them go cold turkey and you don’t have the appropriate medical management, they will transition to illicit street drugs.”

Ground Zero of the opioid epidemic
One of the unique challenges when it comes to preventing addiction among wounded IDF soldiers, according to professionals, is, indeed, at the point of “transfer of care” during the rehabilitation process. As long as the patient is still officially a soldier, he is under the responsibility of the IDF – even if he is being treated at a civilian hospital. As soon as he is released from military service, he is transferred to the care of the Ministry of Defense’s Rehabilitation Department – which means that subsequent medical treatment is split between two parties: for all of his routine medical needs, the patient goes to his HMO, like every other Israeli; for treatment or drugs related to his wounds, any request will be examined by physicians from the Defense Ministry before being approved.
The first stage, during which the wounded soldier is still treated within the military framework, can last several months. According to the IDF, “All soldiers treated with opioids and similar medications are under supervision. Cases where there is suspicion of developing dependence or addiction are handled in consultation with the IDF’s Head of Pain Management, a physician with the rank of Major (Reserves). Painkillers are prescribed as needed, with awareness of the risk of dependence, and doctors may also consult with the Head of Management, in cases where there are disagreements with the hospital’s recommendation.”
In addition, the IDF states that during the war it established a unit called “Continuing with Life,” aimed at supporting injured soldiers throughout their rehabilitation. According to the IDF, “The unit accompanies the wounded and provides emotional and social support through mentors and rehabilitation fellows, most of whom have a background in recovery or relevant life experience, but are not professionals. When medical issues arise—including concerns about addiction to painkillers—the mentors consult with professional staff who operate under the unit.”

The IDF declined to specify how many opioid prescriptions have been issued to soldiers, or how many have received addiction-related support in recent years. Requests to interview relevant officials—such as the Head of Pain Management or the commander of the “Continuing with Life” unit—were also denied. An IDF spokesperson stated: “We place the utmost importance on the physical and mental health of IDF’s wounded and disabled soldiers, and are committed to supporting their rehabilitation process in a comprehensive and personalized manner.”
According to figures issued by the Ministry of Defense’s Rehabilitation Division, obtained by Shomrim and published here for the first time, the number of opioid prescriptions prescribed for wounded soldiers, by the division’s doctors has actually dropped – from 7,637 in 2022 to 6,260 last year. an average of 520 prescriptions a month for 78,000 wounded and disabled veterans under the division’s care.
Officials from the Rehabilitation Division who are familiar with the issue believe there are two factors involved in the decline of opioid prescriptions: the first is a change in attitude toward medical marijuana, which allows long-time patients to exchange their opioid prescriptions for cannabis prescriptions. The second factor is that, while many of the patients wounded in the war have been released from the IDF and are under the authority of the Rehabilitation Division, they are still receiving treatment in hospitals, so they are given opioids there rather than through the Ministry of Defense. If this is indeed the case, there is a massive wave of opioid usage waiting to come out of the hospitals’ rehabilitation wards, since these patients have yet to reach the Rehabilitation Division.
There is certainly good reason to be worried if Israel follows the tragic pattern of the United States. Even within the American population that became addicted to painkillers in massive numbers, veterans are an especially vulnerable group, sometimes referred to as the “ground zero” of the opioid epidemic. Studies conducted over the years have found that the rate of opioid overdoses among veterans far exceeds the rate among the rest of the population.
In Israel, in hospitals’ rehabilitation wards, staff are using various methods to try and prevent addiction and dependence on opioids. Dr. Ofir Morag, the Head of the Cancer Pain Unit at Tel Hashomer and an expert in pain management, says that the hospital has provided physicians and nurses with extra training in the use of opioids. In addition, the Israel Public Health Association has set up a dependency clinic designed to help patients reduce their use of opioids. The clinic employs dedicated clinical nurses with expertise in pain management, who try to balance “controlling the pain and the prudent use of drugs.”
“The clinical nurses are somewhere between regular nurses and doctors,” Morag explains. “She has expanded authority; she doesn’t need a doctor’s approval for everything she does and she decides on the treatment program – with the goal of reducing the consumption of opioids. She has to ensure that the patient is not given too many and that they are administered properly – and, at the same time, start introducing non-opioid drugs, as well as treatments like neural blockades.” These are procedures that interrupt pain signals in specific nerves, like an epidural shot, thereby reducing or eliminating the need for opioids.
“Nowadays, there is a lot more reliance on what we call multimodal treatment,” Morag adds. “Sometimes it can be blockades, for example, but also to bring in a pain psychologist and sit him down next to the patient’s bed. We can also use drugs like ketamine for a very short period of time at a very low dosage. There are drugs that went out of fashion long ago that we are bringing back because we don’t want to use opioids.”
Even before starting opioid treatment, Morag and the other doctors try to identify in advance which patients are more liable to develop a dependency. “If he is keen to take opioids, you know he is in a high-risk group. If he gets high every time he takes a Percocet, you can see it in his behavior. If you identify someone with a high-risk factor, you need to intervene. That could even include contacting the GP and deciding that only one of us will write prescriptions for opioids, to avoid double-dosing.”
Morag says that, when it comes to treating soldiers wounded in the war, “we want to give as few opioids as possible – but, when there’s no choice, we give less dangerous drugs, we reduce the dosages, we’re in touch with the community doctors and when we identify patients more likely to develop dependency we are in much closer contact with them. There’s a blanket policy of not sending anyone home with an opioid prescription; rather, we make a recommendation to the doctor from the Ministry of Rehabilitation Division. I take these things very seriously.”

Drug rehab centers are getting ready
If a patient’s condition deteriorates, the next likely step is admission to a drug rehabilitation center. Conversations with staff at several of these centers reveal that, even 18 months after the outbreak of the war, they have not been overwhelmed with cases involving war-wounded individuals—in fact, they have encountered very few.
Dan Amram is a social worker who works at the Public Health Association’s dependency clinic at Tel Hashomer, where staff work to reduce dependency on painkillers. He also served as a mental-health officer in the IDF reserves for over a year during the war. Amram says that he has just received his first rehab referral for a soldier wounded in this war. “I treated him as a mental-health officer in reserves. I was the one who told him that his friends had been killed. And now I see that he’s the first addicted soldier from this war.”
One explanation for why soldiers are not yet showing up at drug rehab centers is that addiction is a gradual process. It typically begins with physical dependency, where stopping use leads to withdrawal symptoms. Soon after, other signs of addiction often emerge: dropping out of work or school to use, damaged relationships, and more. It usually takes time before a person struggling with addiction seeks help and reaches out to a rehab center.
Amram has a different explanation. “If a soldier comes back from battle and is busy dealing with his pain, it creates a very strong construct of pain in his mind,” says Amram. “So, on many occasions, they will give large doses of painkillers so that the pain does not become chronic. The big problem is that, in the end, you cannot always draw the line between when the soldier is genuinely suffering from physical pain and when he is soothing the emotional pain with opioids. If a soldier says that he is in pain, no doctor in the world can tell if he’s really suffering because he saw four of his friends killed in the same incident he was wounded. So, they just go with the flow – and they are still in the first stages. I believe that they are a little scared of the moment that they will have to reduce the dose of opiates and start dealing with the physical and emotional pain – and all that entails.”
Amram says that there is another factor, too: the huge pressure on systems that are not used to dealing with so many wounded people. “I walked around the hospitals and I saw the huge burden on the healthcare system in the face of the fighting,” he says. “This is not a routine situation in which one specific soldier was wounded. So, what’s keeping it all together for now? Opioids.”